Raw tuna. Copious caffeine. Cigarettes. Unpasteurized brie. Alcohol.
Most women know to avoid these potentially harmful substances while pregnant, plus certain risky activities such as rock climbing, ice skating, and skiing.
But what if your job could negatively impact your pregnancy?
That’s what a team of researchers from Harvard Medical School and the University of Kansas recently set out to investigate. To start, they narrowed in on expecting mothers in two careers that demand long hours: medicine and law. But physicians — surgeons, in particular — spend many of those hours on their feet, often facing life-or-death stakes. The team wanted to know: Does that extra stress lead to negative birth outcomes, including shorter pregnancies, lower birth weights, premature births, and even health issues for newborns?
“Anything that a mother experiences during their nine or 10 months of pregnancy can have a lasting impact.”
Lilly Springer, study co-author
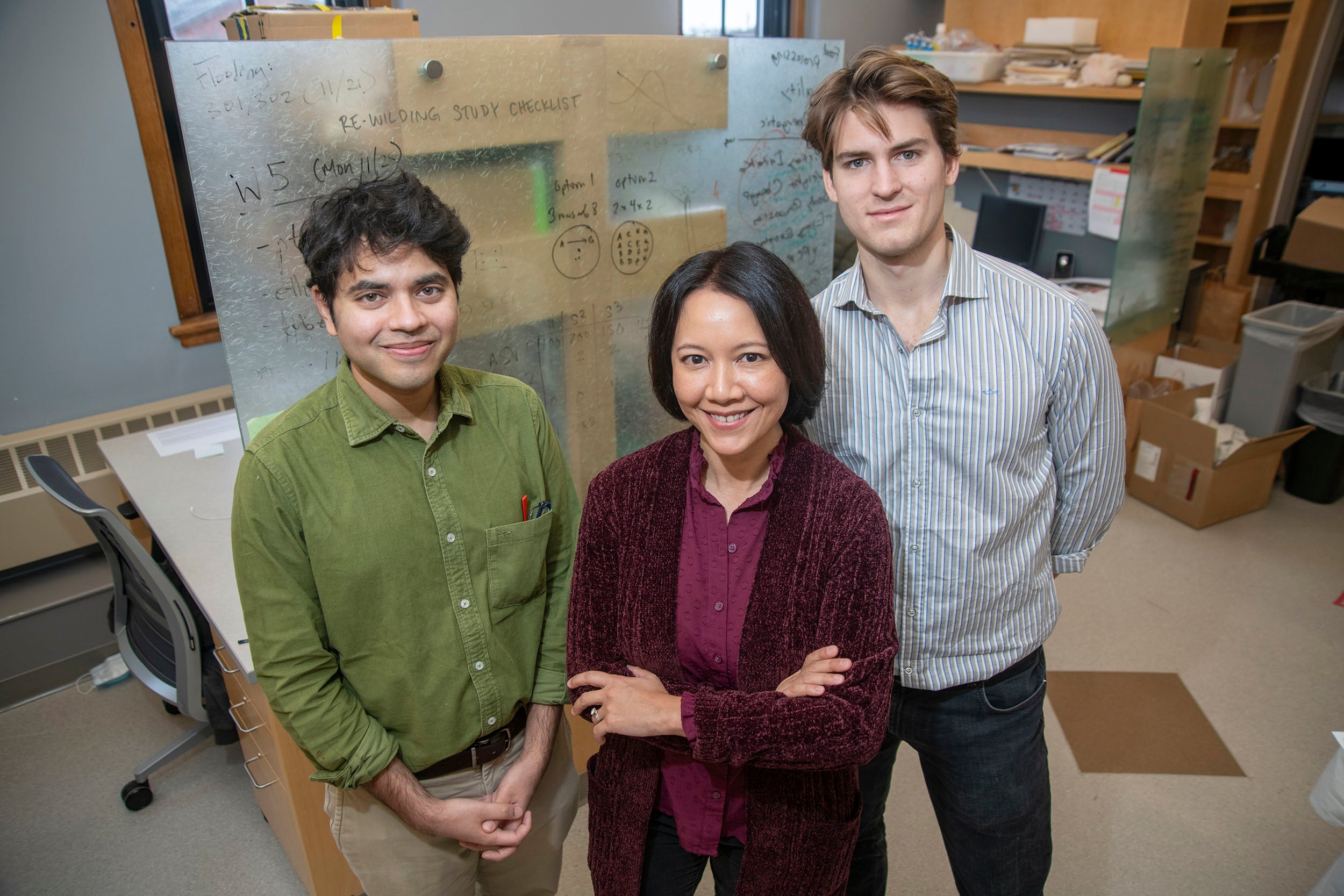
According to the team’s recently published National Bureau of Economic Research working paper, the answer is yes. But the effects are “not enormous in magnitude, which I think is very reassuring,” said Anupam B. Jena, the Joseph P. Newhouse Professor of Health Care Policy at the Medical School, associate physician at Massachusetts General Hospital, and one of the authors on the paper.
The paper, which was co-authored by David Slusky, a professor of economics at the University of Kansas, has not yet been peer-reviewed.
“It certainly does suggest that there might be some differences in birth outcomes that are attributable to the lifestyle of medicine, all the things that it includes,” Anupam said. “But it’s also important not to sell it to be more than what it is.”
The correlation between stress and pregnancy problems is well documented. One study found that in the six months after the Sept. 11 attacks, women with Arabic names experienced a 34 percent increased chance of their baby being born with a low birth weight. The authors pinned that increase to a surge in anti-Arab sentiment, which elevated the women’s stress levels.
But even seemingly more benign events that are dramatic and unexpected, like your team winning the Super Bowl, led to a 4 percent increased likelihood of a low birth weight, according to another study.
“Anything that a mother experiences during their nine or 10 months of pregnancy can have a lasting impact on not only the immediate birth outcomes, but adolescence, and even young adulthood,” said Lilly Springer, a Madison & Lila Self graduate fellow at the University of Kansas and an author on the paper. “Those nine months are incredibly formative.”
According to the paper, physicians tend to have about 2.3 percent lower birth weights and 0.3 percent shorter pregnancies than lawyers; surgeons fare a bit worse in pregnancy length (about 0.9 percent shorter) and are about 32 percent likelier to deliver prematurely than non-surgeon physicians. Anupam said these numbers are not extreme. They’re comparable to the effect of air pollution on infant health.
2.3%
Lower birth weights for physicians than lawyers, according to the study
But for some expecting mothers, even a small reduction in their infant’s birth weight could be cause for concern.
“Two percent doesn’t seem like a big deal,” Springer said. That’s only a third of the birth weight gap between Black and white mothers. But it’s bigger than the education and urban-rural birth weight gaps. And if an infant is hovering around a riskier weight (typically under 5.5 pounds), “a 2 percent difference can really push you over the edge,” Springer said.
But both Springer and Anupam want to make it clear: These results do not mean that expecting mothers should avoid high-stress jobs or quit when they get pregnant (which, for many, isn’t a viable option anyway). Nor should the findings provide a rationale to discriminate against women, blocking them from entering high-stress careers.
“It’s really easy to look at the study and say, ‘Well, physicians shouldn’t get pregnant, or women shouldn’t have children if they’re in a very stressful environment,’” Springer said. “That is a knee-jerk reaction. But that would be a disservice to everyone.”
Instead, the team hopes these findings lead to further studies that examine how specific hospital environments — and their gender ratios, policies on parental leave, required hours, and even prevalence of sexism — might be impacting their pregnant staff members.
As part of their study, the researchers analyzed the impact of two workforce reforms (in 2003 and 2011), which limited the number of hours physician trainees could work. Although they found a negligible impact on birth outcomes, this shift was too minor and impacted too small a cohort to make any sweeping conclusions. But the team does see workforce reform as a potential solution for physician mothers. Many women surgeons report experiencing high levels of sexism, which can add to their overall stress. And some hospitals don’t offer accommodations to help expecting parents reduce their stress levels while continuing to work. These issues can be fixed.
But because expecting mothers cannot always control their work environment, Springer thinks it’s critical that mothers at least understand the potential risk their jobs could pose to their pregnancies.
“Unfortunately, in the United States, pregnant women, especially Black pregnant women, have to be advocates for themselves,” Springer said. She recommends pregnant women talk to their doctors about their jobs.
This risk might not be limited to physicians and surgeons. The team launched their exploration by focusing on a typically well-educated, higher-income population, which is likelier to have access to high-quality healthcare and inherent knowledge about their health. Because those qualities are often associated with more positive birth outcomes, these effects could potentially be lower than other physically demanding or high-stress jobs, like fast food workers, firefighters, or even delivery truck drivers — one group Springer would be curious to examine further. The team’s current Texas dataset has this bonus: Demographically, Texas is like a mini U.S. That makes it more reasonable to extrapolate any results to the broader country.
Next, the team is planning to refine and publish their results, use the Texas dataset to explore other maternal questions, and potentially analyze how specific hospital environments could contribute to negative birth outcomes for physician mothers.
“The take-home is actually if there is an impact on infant health, we should figure out how to mitigate that,” Anupam said. “The idea here is to figure out how you can do something right and do it safely.”